18 children were injured, some critically, in the recent Christmas parade attack in Waukesha, Wisconsin.
Local news is reporting that Wisconsin’s largest Children’s hospital is having a difficult time caring for these children due to medical staff shortages caused by a COVID-19 vaccine mandate, and their refusal to honor most religious exemption requests.
Wisconsin’s largest children’s hospital has been struggling to care for patients in the wake of the Waukesha Christmas Parade attack in large part because of staffing issues stemming from its COVID-19 vaccine mandate, multiple sources tell “The Dan O’Donnell Show.”
18 children were brought to the Children’s Wisconsin Milwaukee Hospital with injuries suffered when a driver plowed into parade-goers Sunday afternoon. One of those children was among the six people killed when he succumbed to his injuries Tuesday afternoon. Several of the young victims remain in critical or serious condition, and sources say the hospital simply did not have enough nurses or support staff to adequately handle the sudden rush.
“It was a nightmare,” said one nurse, who spoke on condition of anonymity because she is not authorized to speak on the record. “We just don’t have enough people and [supervisors] were frantically calling in everyone they could, but it wasn’t enough. We are taking care of everyone the best we can, but it’s hard.”
A high-ranking official at Children’s, who also spoke on condition of anonymity, said the hospital currently has hundreds of open positions and attributes much of the staffing shortage to the COVID-19 vaccine mandate.
The Children’s Wisconsin website lists 239 open positions at its Milwaukee hospital and more than 450 across all of its campuses.
Religious exemption requests were due September 15, and The MacIver Institute reported that more than 70 percent of them were denied.
On October 14, Children’s was forced to close its Delafield clinic until the end of December because of severe staffing shortages.
“This is because of the mandate,” one source said flatly. “People either quit because their exemptions were denied or didn’t even bother to apply. They just started looking for other jobs.”
A nurse who was working Sunday night said the staffing shortage was so severe that even Children’s President and CEO Dr. Peggy Troy was working the Emergency Department floor.
“I know it was partly ceremonial to say ‘We’re all in this together,’ but it was also because we just needed all the help we could get,” the nurse explained. “Dr. Troy was there until at least 2 am.”
The shortages continue, the nurse said, and are so severe that she and other nurses who volunteer to work an additional 12 hours over the Thanksgiving holiday weekend will be given $4,500 bonuses.
The hospital official confirmed that administrators were giving out $1,000 bonuses to get nurses and other employees to work Sunday night into Monday morning.
Children’s Wisconsin has not yet responded to a request for comment on its staffing issues or the desperate measures it has undertaken to deal with the sudden influx of new, seriously injured patients.
This nursing shortage is not unique to Children’s, as hospitals across the country have reported significant issues since the beginning of the COVID-19 pandemic. However, the issue seems to have been dramatically exacerbated once hospital systems began requiring employees to be vaccinated. (Source.)
This follows a trend nationwide where Emergency Rooms are beginning to close down due to staffing issues and so many medical staff being fired or quitting due to the COVID-19 vaccine mandates.
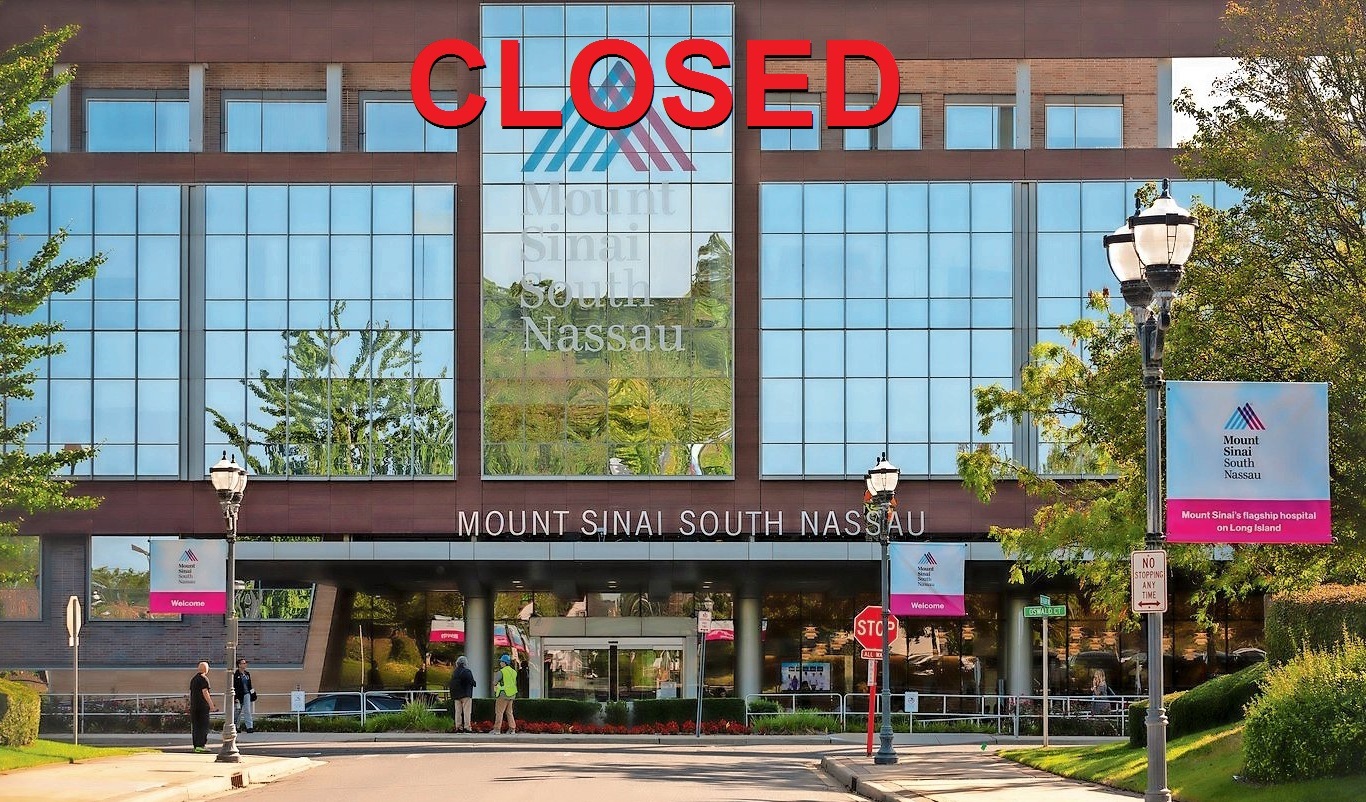
This week it was announced that Mount Sinai South Nassau-operated Long Beach Emergency Department in New York was forced to close after more than 70 of their staff who had “temporary religious exemptions” to the COVID-19 vaccine mandate were denied their exemptions and fired.
The Mount Sinai South Nassau-operated Long Beach Emergency Department was forced to close Monday afternoon due to nursing staff shortages occurring as a result of the state vaccine mandate, according to the hospital.
The decision to temporarily close the facility, the only emergency room in the 50,000 resident city of Long Beach, was made after all other options were exhausted, according to the hospital.
A hospital official said an ambulance will be stationed around the clock at the closed location for the duration of the closure to take patients in need of emergency care to the hospital’s main campus in Oceanside — a trauma center designated facility five miles away, which takes about 15-20 minutes to reach by car.
The hospital said that the staffing shortage and subsequent closure is a result of the hospital’s compliance with the NYSDOH’s mandate issued Thursday which requires the suspension of any staff working under temporary religious exemptions who cannot show proof of receiving a first dose of COVID-19 vaccination or a valid medical exemption from receiving it.
The hospital lost six dozen employees. According to the hospital, all were unvaccinated but working with a religious exemption — an exemption that ended last week. Some of these six dozen employees are ER nurses who the hospital said are not easily replaced due to training and other factors, the hospital went on to say.
The New York State Department of Health (NYSDOH) was notified of the need to close the free-standing Long Beach Emergency Department (LBED) on Friday and granted verbal approval, according to Mount Sinai South Nassau. The emergency department, which sees about 10,000 visitors annually, will be closed for at least a month.
Here are some more media reports of ERs and hospitals closing down around the country due to staffing shortages.
ED service to remain closed at Catholic Health Orchard Park center amid staffing shortages
Catholic Health’s Mercy Hospital of Buffalo (N.Y.) will keep the emergency department at the Mercy Ambulatory Care Center in Orchard Park, N.Y., closed for the next several weeks, the health system announced Nov. 18.
Nursing shortage forces Syracuse’s biggest hospital system to shut down 20% of patient beds
Upstate University Hospital has temporarily closed 124 beds because it doesn’t have enough nurses to care for patients.
That means nearly 20% fewer beds are available at Syracuse’s largest hospital that cares for some of the sickest and most seriously injured patients in a 14-county area.
Minnesota hospitals get federal help to address staff shortages
Federal medical teams will arrive in Minnesota next week to provide much needed staffing support at two state hospitals hit hard by the ever-growing COVID-19 surge.
HCMC and CentraCare, including St. Cloud Hospital, each will receive 22 emergency medical workers from the Department of Defense after a request from Gov. Tim Walz.
While many of these reports are blaming “outbreaks of COVID-19” for the staffing shortages, NPR recently reported that many of these ERs are “swamped with seriously ill patients” who “don’t even have COVID.”
Inside the emergency department at Sparrow Hospital in Lansing, Mich., staff members are struggling to care for patients who are showing up much sicker than they’ve ever seen.
Tiffani Dusang, the emergency room’s nursing director, practically vibrates with pent-up anxiety, looking at all the patients lying on a long line of stretchers pushed up against the beige walls of the hospital’s hallways. “It’s hard to watch,” she says in her warm Texan twang.
But there’s nothing she can do. The ER’s 72 rooms are already filled.
“I always feel very, very bad when I walk down the hallway and see that people are in pain or needing to sleep or needing quiet. But they have to be in the hallway with, as you can see, 10 or 15 people walking by every minute.”
It’s a stark contrast to where this emergency department — and thousands others — were at the start of the coronavirus pandemic. Except for initial hot spots like New York City, many ERs across the U.S. were often eerily empty in the spring of 2020. Terrified of contracting COVID-19, people who were sick with other things did their best to stay away from hospitals. Visits to emergency departments dropped to half their normal levels, according to the Epic Health Research Network, and didn’t fully rebound until the summer of 2021.
But now, they’re too full. Even in parts of the country where COVID-19 isn’t overwhelming the health system, patients are showing up to the ER sicker than they were before the pandemic, their diseases more advanced and in need of more complicated care. (Full story.)
The “elephant in the room” that nobody in the corporate media dares to report, of course, is that the vast majority of these patients are vaccinated, and suffering from COVID-19 vaccine injuries.
And with the FDA now authorizing a 3rd COVID-19 “booster shot” from Pfizer and Moderna, we can expect this situation to only get worse, especially when the children between the ages of 5 and 11 who are just now being injected start to experience these COVID-19 vaccine injuries.
In the UK, which also authorizes the Pfizer and Moderna COVID-19 shots, public health statistics now show that 89% of COVID-19 reported deaths are among the fully vaccinated, and that those vaccinated with these experimental shots are more likely to die with a COVID-19 diagnosis. (Source.)




 Loading ...
Loading ... 
